PODOCONIOSIS
(Endemic elephantiasis, Non-filarial elephantiasis, Big foot disease, Idiopathic elephantiasis, Microcrystal disease, Mossy foot, Lymphostatic verrucosis)
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it
Podoconiosis (from the Greek podos, foot and konia, dust) is a non infectious and not contagious disease (not triggered by any bacterium, virus or parasite) that manifests itself as a massive swelling (elephantiasis) of the feet (especially) and legs, which leads to disfigurement and disability. It was classified as a Neglected Tropical Disease (NTD) by the World Health Organization in 2011. Podoconiosis (or simply “podo”) is a disease of the lymph vessels of the lower extremities. It is the second most common cause of tropical lymphedema after filarisis. It is commonly called Mossy Foot disease because its occurrence results in skin that becomes very rough and bumpy and changes to look like moss.
It is found in the tropics in Africa (Ethiopia, Cameroon, Rwanda, Burundi, Uganda, Tanzania, Kenya, Sudan, and the islands of Cape Verde, Bioko, Sao Tome & Principe), central America and Asia.

It is caused by prolonged exposure to irritant minerals in red clay soils (the reddisch-brown rusty color of the soil is an expression of the high iron content).

Podoconiosis is mostly a disease of agrarian people who work barefoot in the fields, notably on red clay soils in upland volcanic areas, either inactive or active, especially at altitudes around 1500 m. (5,000 ft) (mean altitude of 1225 masl). The altitude ensures enough rainfall (mean >1500 mm annually), at suitable temperature (mean annual LST 19-21°C), to produce weathering of rocks and so a fertile soil.
It is estimated that Ethiopia has the highest total number of cases per country because the soil type thought to be associated with the disease covers approximately one-fifth of the country and the fertility of the soil in such areas attracts an agricultural population.

Individuals afflicted with podoconiosis suffer debilitating physical effects, including attacks when the leg becomes warm, painful and even more swollen, and are ostracized from their communities because of misconceptions about the cause of podoconiosis. Men and women are equally affected. Onset of symptoms is in the first or second decade with a progressive increase in podoconiosis prevalence up to the sixth decade. Farmers who for cultural reasons or through sheer poverty do not wear shoes are at high risk, but the risk extends to any occupation with prolonged contact with the soil. Ernest W. Price, a British surgeon living in Ethiopia correlated, in the 1970s and 1980s, the origin of 800 patients who attended as elephantiasis clinic in Addis Ababa with various data (climate, altitude, vegetation, population, genetics, geology), locating on a map of the country. In the area of prevalence he noted that the disease was limited to the barefoot section of the community and closely related to the extent of the “tropical red soil” developed from the basalt.
The distribution of the disease suggested the discovery of the true etiology of podoconiosis: the association of endemic elephantiasis of the lower legs in East Africa with soil derived from floods of lava (notably basalt). Using light and electron microscopy he discovered kaolinite in the phagosomes of macrophages in the femoral lymph-node. Price demonstrated that the lymphatic vessels of the patient affected by podoconiosis experienced subendothelial edema and subsequent collagenization of the lumen that is finally entirely obliterated
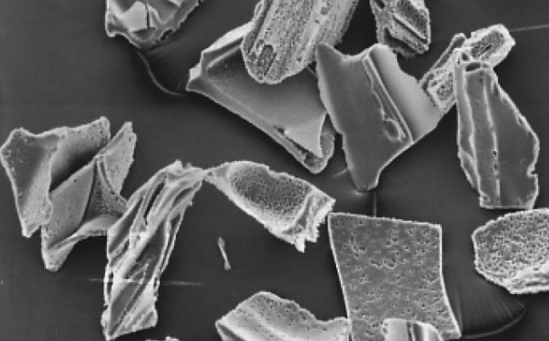
Lava in the above climatic factors (altitude and warm rainfall) disintegrates steadily (predominantly iron oxide, alumina and silica) and reconstitutes into more stable silicate clay minerals (notably kaolinite) composed of small crystals in colloid size, with maximum length of 2 microns, and the hydroxides of iron and aluminium.
The red-brown, slippery and sticky clay adheres firmly when wet to the skin of feet and lower legs of the agricultural workers. Mineral analysis of the soil in some areas of high prevalence of podoconiosis, revealed high values of zirconium (Zr) and beryllium (Be), known for their ability to induce granuloma formation in the lymphoid tissue and doubtlessly a factor involved in the development of lymph node sclerosis leading to elephantiasis.
Clay particles enter through cracks and fissures in the skin of the foot and are taken up into macrophages in the lower limb lymphatic system. These particles then appear to react directly with lymphatic vessel walls, leading to failure of the lymphatic system in the lower legs, chronic inflammatory response (endolymphangitis), obliteration of the lymphatic lumen and elephantiasis. Not everyone who lives and works on irritant soils without shoes becomes affected. Studies have shown that podoconiosis is the result of a genetically determined abnormal inflammatory reaction (podo susceptibility) to mineral particles in soil derived from volcanic deposits. Furthermore long term exposure is necessary. So tourist will not be affected. Podoconiosis is characterized by a prodromal phase before elephantiasis sets in.
Prodromal symptoms commonly include
- itching of the skin of the forefoot and
- burning sensation in the foot and lower leg.
“Itchy foot” is a persistent localized itching, usually on the dorsum at the base of the first or second toe clefts, or below the middle malleolus. From constant scratching skin can become thickened (pachydermia) “Burning leg”: it’s a burning sensation in lower leg, worsening at night, usually the same leg at each episode. Nocturnal leg and foot pain in a young person is a classic feature. The second leg does not usually become involved until the first one shows clear signs of disease.
Early changes that may be observed are
- splaying of the forefoot,
- plantar oedema with lymph ooze,
- increased skin markings,
- pachydermic forefoot,
- ‘block’ (rigid) toes.


''Splayed forefoot' is a widening of the forefoot, and separation of the toes, which gives the foot a spatula-like appearance, on one or both sides. It is due to deep edema between metatarsal heads.
Plantar edema is asymmetrical (unlike cardiac or renal edema). A simple test is to press with the thumb on the sole over the head of the first metatarsal: it is possible to see mild lymphatic oozing, tiny blebs of lymph or an unusual number of flies attracted to it.
Increased skin markings at the base of the first toe cleft and running longitudinally rather than laterally (as is normal).
Pachydermic (thickened) forefoot shows an hyperkeratosis (excessive deposit of keratin) on the dorsum at the base of the first or second toe cleft. The clefts themselves usually remain normal, even in advanced disease.
''Block rigid toes' lack their normal curves, and look wooden and rigid, as if they were nailed on the forefoot.
Later, the swelling may be one of two types: soft and fluid (‘water-bag’ type, left figure) or hard and fibrotic (‘leathery’ type, often associated with multiple hard skin nodules, right figure).

Very long-standing disease is associated with fusion of the interdigital spaces and ankylosis of the interphalangeal or ankle joints . Finally leg becomes “mossy” and nodular, lymph may ooze through the skin, which may be secondarily infected by fungi or bacteria.
The disease may progress steadily, or there may be a succession of acute episodes in which the patient is pyrexial and the limb warm and painful that resolve incompletely. These episodes appear to be related to progression to the hard, fibrotic leg. Differential diagnosis is based first of all on location, history and clinical findings.
The two conditions must most often be distinguished from podoconiosis are:
filarial lymphedema (FL) and leprotic lymphedema.
Filarial lymphedema
The outward appearance of legs and feet affected by podoconiosis and lymphatic filariasis is very similar. Some questions to the patient can help to decide the correct diagnosis. If the patient lives more than about 1,500 metres (5,000 ft) above sea level, the leg swelling is likely to be due to podoconiosis, because the mosquitoes that transmit lymphatic filariasis usually do not survive above this altitude (it is too cold at night), even if a recent work ( Shiferaw W. et al, 2012, Trans R Soc Trop Med Hyg 106: 117–127) documented lymphatic filariasis in areas up to 1698 masl. If the patient does not live in zones where lymphatic filariasis is known to be prevalent, the diagnose should be podoconiosis. If it started in the feet and both feet/legs are affected (though asymmetric) and ascending but not above the knee, then the diagnosis is likely to be podoconiosis. If the swelling tend to start in the groin and spread downwards the feet, if swelling is predominantly unilateral (in one leg), if the swelling is extended above the knee, and/or the lymph nodes in the groin are enlarged, the disease is likely to be lymphatic filariasis. Laboratory test (anti-filarial antibody examination) can be used to distinguish podoconiosis from LF where clinical diagnosis is problematic.
Leprotic lymphedema
Podoconiosis may be distinguished from leprosy lymphoedema by
- the preservation of sensation in the toes and forefoot,
- the lack of trophic ulcers,
- thickened nerves or hand involvement.

Another possible cause of lymphedema is mycetoma pedis. Mycetoma is a chronic, granulomatous disease of the skin and subcutaneous tissue due several fungi (when is called eumycetoma) or actinomycetes (called actinomycetoma), bacteria that produce filaments, like fungi.
It affects usually the foot. It is common among young adults (more males than women, aged between 20 and 40 years) who walk barefooted, commonly farm workers, exposed to acacia trees or cactus thorn pricks containing the etiologic agent that normal live as saprophytes. Mycetoma is endemic around the Tropic of Cancer (15°south and 30° north of the equator)(“Mycetoma belt”).
It is characterized by a painless firm swelling (tumefaction) of the affected area with a skin darker and firmer than the surrounding tissue and in a later phase nodules, abscesses and fistulae draining a clear viscous or purulent exudates. Podoconiosis has a mossy appearance that mycetoma has not, edema of podoconiosis is tipically more striking and extends more prossimally than the edema of mycetoma.
Podoconiosis is typically found in higher altitude areas with vulcanic soil, whereas mycetoma is found along the “mycetoma belt”. If diagnosis is questionable, radiology can help distinguish between the two diseases, because mycetoma can invade the bones.
Prevention of podoconiosis is based on three stages.
Primary prevention consists of protection of the feet, avoiding or minimizing prolonged exposure between the skin and irritant soils by regular use of robust footwear (shoes or boots) and by covering of floor surfaces inside traditional huts in areas of irritant soil.
Secondary prevention (prevention of the progression of early symptoms and signs to overt elephantiasis) consists of training in foot hygiene (includes daily washing with soap, water and antiseptic, use of emollients), compressive bandaging in selected patients (soft type of swelling) before rising in the morning (with an ankle-length elastic socks or with a wide -10 cm- one-way stretch elastic bandages), elevation of the leg, controlled exercises (to improve the circulation, such as toe points, ankle circles and calf raises, two or three times per day), and use of socks and shoes. Compression bandaging is highly effective in reducing the size of the soft type of swelling (patient shown before at left and after 6 months of treatment at right).


Tertiary prevention (cases with advanced elephantiasis) encompasses secondary prevention measures (elevation for at least 18 hours with the legs at or above the level of the heart are needed each day and twice daily compression with elastic bendages of the affected leg or intermittent compression machine if electricity is available), plus, in selected cases, nodulectomy (removal of prominent nodules) Social and spiritual rehabilitation is vital to
- restore a sense of worth and community,
- diminish family and community stigma,
- train treated patients in skills that enable them to generate income without contact with irritant soil.
