Acute generalized exanthematous pustolosis (AGEP)
Luciano Schiazza M.D.
Dermatologist
c/o InMedica - Centro Medico Polispecialistico
Largo XII Ottobre 62
cell 335.655.97.70 - office 010 5701818
www.lucianoschiazza.it

Acute generalized exanthematous pustulosis (AGEP) is an uncommon cutaneous pruritic eruption which is characterized by acute, rapid onset of numerous (dozens to hundreds to thousends) of small, pinhead-sized, sterile, superficial (located subcorneally in the epidermis), non-follicular pustules that arise on erythematous and edematous skin. AGEP was first described in 1980 by Beylot et al. and named, in French, pustuloses exanthématique aiguës généralizés (PEAG). The eruption usually begins on the face and in the main intertriginous regions where is often accentuated.
The patient commonly manifests:
-
Fever
-
Elevated numbers of blood neutrophils
Mucous membrane involvement may occur in about 20% of the cases but usually is mild and remains limited mostly to oral location.
After resolution of pustules a characteristic collarette-like postpustular desquamation can be seen.
AGEP may have other systemic manifestations, such as renal failure, hyperthermia, lab abnormalities, and/or hemodynamic instability,
Most cases of AGEP are often provoked by drugs, particularly by antibiotics and mainly beta-lactams.
But the list of drugs responsible of AGEP is increasing:
-
Aminopenicillins,
-
Macrolides,
-
Terbinafine,
-
Itraconazole,
-
Betalactams,
-
Doxycycline,
-
Nystatin,
-
Furosemide,
-
Calcium channel blockers,
-
Analgesics,
-
Anti-pyretics,
-
Paracetamol,
-
Dexamethasone solution,
-
Tyrosine kinase inhibitor STI571 (anticancer drug),
-
Salazosulfapyridine,
-
Valdecoxib,
-
Metronidazole,
-
Clindamycin,
-
Nimesulide,
-
Phenobarbital.
Sulfonamides are notably not a frequent cause of AGEP
Few cases are related to other causative factors as
-
acute infections with enteroviruses,
-
hypersensitivity to mercury,
-
ultraviolet radiation,
-
spider bites.
The treatment is simply stopping the offending drug: after withdrawal of the causative drug generally AGEP usually resolves within a few days (approximately 2 weeks) without specific treatment with the only sequelae of generalized desquamation. Sometimes, because of the patient's age and co-morbidities, symptomatic treatment (antipyretics, antipruritics, intravenous and topical steroids and emollients) is required.
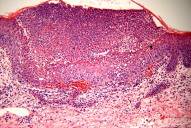
Histologically, AGEP may demonstrate subcorneal pustules with a background of dermal edema and spongiosis, leukocytoclastic vasculitis, perivascular eosinophils, and focal necrosis of keratinocytes with negative immunofluorescence.
AGEP can be considered a reaction pattern.
Pustular skin disorders need several differential diagnosis. In the etiology of cutaneous pustular eruptions it is important to consider the distribution of the lesions and the age of the patient.
AGEP is characterized by:
-
short time to onset in response to the administration of the suspected drug (less than 24 hours in most cases)
-
antibiotics as causative agents in 80% of cases.
Some disseminated eruptions require differentiation from AGEP:
-
pustular psoriasis (von Zumbusch type),
-
subcorneal pustular dermatosis (Sneddon-Wilkinson disease),
-
IgA pemphigus,
-
drug rash with eosinophilia and systemic symptoms (DRESS),
-
toxic epidermal necrolysis (TEN).
The major way to separate AGEP from pustular psoriasis is:
-
family history of psoriasis,
-
way of presentation,
-
psoriatic features such as nail changes,
-
geographic tongue,
-
characteristic arthritis,
-
involvement of palms and soles,
-
sparing of the face, skin histopathology,
-
exposure to drugs.
From ingestion of drug and beginning of AGEP the median time is 1 day. AGEP also has shorter duration of pustules, fever, and less severe systemic involvement. Lithium and beta-blockers can induce pustular psoriasis flares, but not AGEP.
Subcorneal pustular dermatosis (Sneddon-Wilkinson disease) can also present with a disseminated pustular rash. The patient is afebrile and the disease has cyclic reurrence of large, localized, flaccid pustules which usually start in the flexures. Histopathology shows a sterile subcorneal pustule with acantholysis only in older lesions and no spongiosis.
IgA pemphigus is a vesiculopustular, intraepidermal blistering disease. The vesicles are flaccid and disposed in an annular pattern. Direct immunofluorescence is positive with IgA binded to keratinocytes. There aren’t any systemic symptoms.
Drug rash with eosinophilia and systemic symptoms (DRESS) is a systemic drug eruption, with a less pronounced pustular component than AGEP.
In DRESS there are also:
-
lymphadenopathy,
-
eosinophilia,
-
severe visceral involvement (hepatitis, nephritis, pneumonitis, with or without myocarditis).
Toxic epidermal necrolysis (TEN) compared to AGEP has similar history, types of associated drugs (but AGEP is more frequent with aminopenicillins, while TEN is associated more often with sulfonamide antibiotics), and immunology. TEN has significant mucosal involvement, full thickness epidermal necrosis, and Nikolsky's sign (traction pressure on skin can lead to epidermal sloughing).
In neonates, pustules can be a manifestation of sepsis or other serious infectious diseases.
Non infectious generalized pustular eruptions in neonates include:
-
erythema toxicum neonatorum,
-
transient neonatal pustular melanosis,
Pustules are also seen in infants with:
-
congenital cutaneous candidiasis, which may or may not involve disseminated disease.
-
Ofuji's syndrome, an uncommon generalized pustular dermatosis of infancy associated with eosinophilia,
-
scabies infestations.
In AGEP patch tests show strongly positive pustular reactions to suspected drugs, usually after 48 hours of application.
